Medicare Supplement plans are standardized across all states, however, some states have specific enrollment rules and guidelines! This video will review state-specific guidelines for states in New England and the Northeast!
New England Medicare
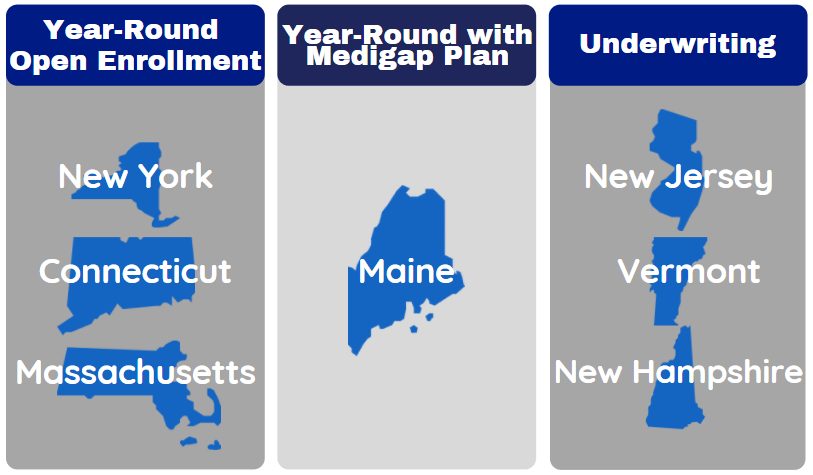
Medicare Supplement plans are standardized across 47 of the 50 states. This means that a Plan G has the exact same benefits, regardless of the state you live in. States and insurance companies are not allowed to alter the benefits offered by the Medigap plans. Each state, however, is allowed to constitute state specific enrollment rules for anyone enrolling in a Medicare Supplement plan more than 6 months past their Part B effective date. Depending on which state you live in, there may be year-round open enrollment, year-round open enrollment with specific criteria, or medical underwriting required to enroll or change plans.
Medicare in New York, Massachusetts and Connecticut
Medicare enrollment in New York, Massachusetts, and Connecticut are very similar. Every state and insurance company required automatic acceptance into a Medicare Supplement plan within the first 6 months of Part B enrollment. This means that there are no health questions to enroll in Medigap plans as long as you are within the first six months of your Part B enrollment.
New York, Massachusetts, and Connecticut take this open enrollment one step further! There is never any medical underwriting required to enroll into a Medigap plan in these states. This means that Medicare beneficiaries can apply for a Medicare Supplement plan during any month of the year, and not be denied for pre-existing conditions or prescription drug history. Medicare beneficiaries are guaranteed acceptance into Medicare Supplement plans in New York, Massachusetts, and Connecticut. This is extremely beneficial, as you are able to always obtain coverage, as well as maintain the ability to change plans based on premiums.
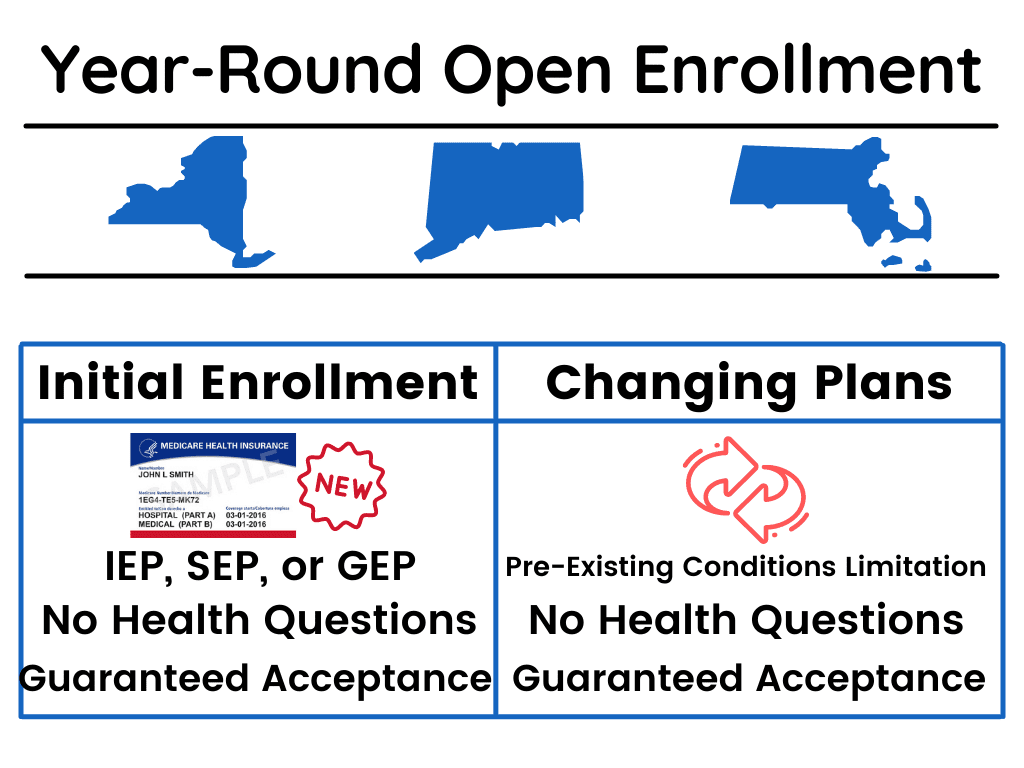
Although you are guaranteed acceptance to these plans regardless of health history, this does not mean that you should wait until the last minute to enroll into a plan. Insurance carriers often have the ability to impose pre-existing conditions limitations for periods of 3-6 months, where there is limited coverage initially if you are not coming from another form of creditable insurance (another Medicare Supplement, Medicare Advantage Plan, or employer-sponsored insurance).
Medicare in Maine
Just like in New York, Massachusetts, and Connecticut, Maine is required to offer open enrollment into Medicare Supplement plans for the first 6 months of your Medicare Part B effective date. In Maine, once you are more than 6 months past your Part B effective date, there is a year-round open enrollment, but it does come with stipulations.
In order to utilize year-round open enrollment for Medicare Supplement plans in Maine, you must already be enrolled in a Medicare Supplement plan. Essentially, in order to change to another Medigap plan with no medical underwriting, you must be coming from a Medigap plan already. Further, you can only use this open enrollment to change to another plan of equal or lesser coverage. This mean you can change from a Plan G to another Plan G, or a Plan G to a Plan N, but you cannot change from a Plan N to a Plan G without medical underwriting.
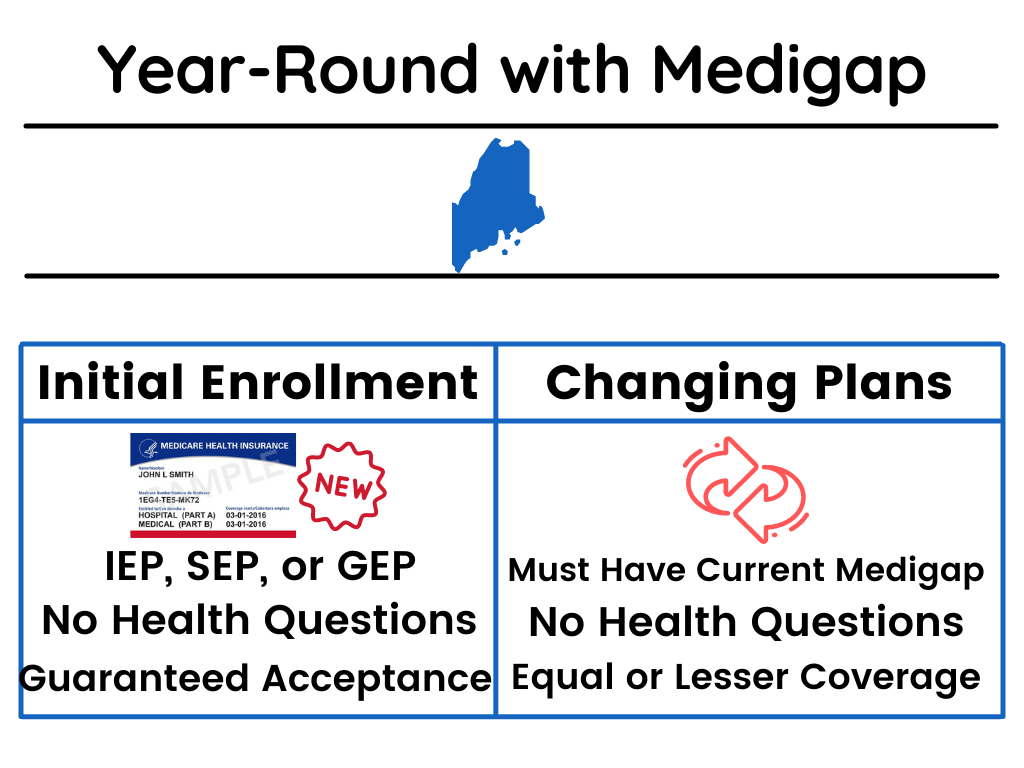
The other state specific Medigap rule that Maine enacts is related to Medicare Supplement Plan A. Insurance carriers are required to offer Medicare Supplement Plan A once per year for anyone to apply for, regardless of health history. This is known as guaranteed issue period. There is a catch, however. The insurance carriers are given the option to choose which month of the year to offer this enrollment. Luckily, insurance carriers must accept you into a Plan A during that month, but Plan A is your only option if you use this guaranteed issue rule in Maine.
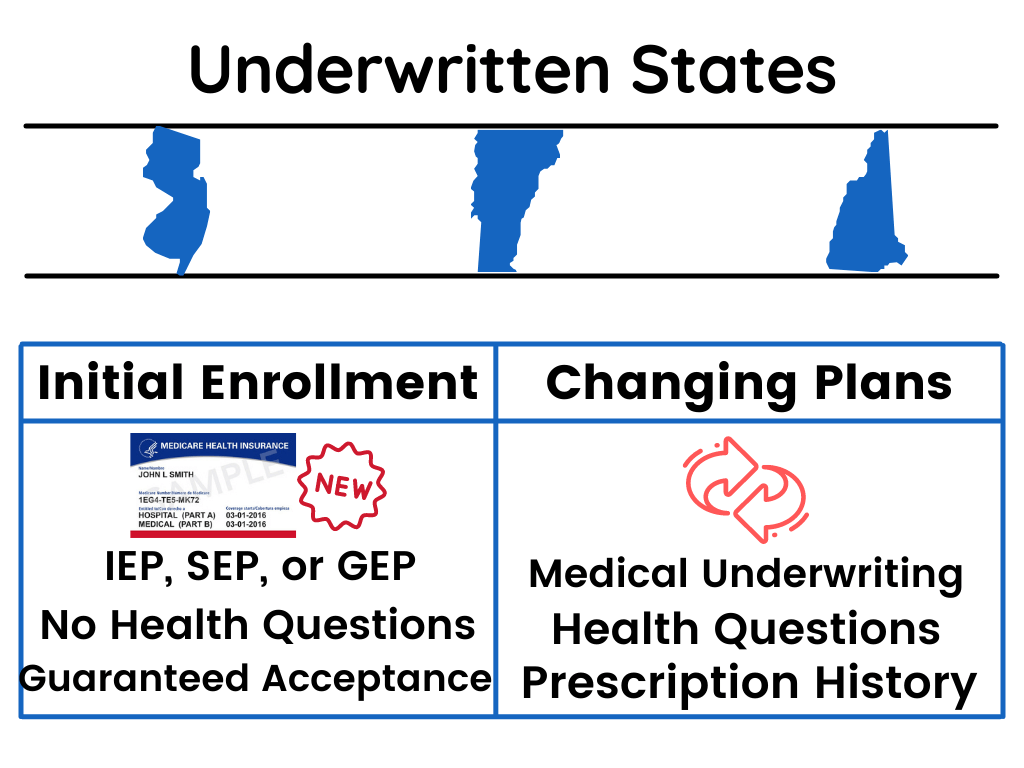
Medicare in New Jersey, New Hampshire, Vermont, and Most Other States
New Jersey, New Hampshire, and Vermont follow the same guidelines as most states in the country. These state are required to offer open enrollment and guaranteed acceptance into Medicare Supplement plans within the first 6 months of your Medicare Part B effective date. Unlike the other Northeastern states, however, the open enrollment for Medigap plans in these states stops there.
The states of New Jersey, New Hampshire, and Vermont required medical underwriting to change or enroll in Medicare Supplement plans once you are 7 or more months past your Medicare Part B effective date. This means that insurance carriers are able to assess your health, prescription drug, and hospitalization history. From this assessment, these carriers are able to either accept you into a Medicare Supplement plan, or deny you coverage.
The majority of states across the US follow these medical underwriting guidelines for enrolling into a Medicare Supplement plan 7+ months past your Medicare Part B effective date.
Medicare By State
Have more state specific Medicare questions? Visit our Medicare By State page and click on your specific state to learn all of your state specific guidelines! Give us a call at 877-885-3484 and an experienced agent will walk you through everything you need to know about setting up your Medicare enrollment!