As a Medicare beneficiary, you want to keep an eye on your mailbox every fall! During the month of September, you will receive a Medicare Annual Notice of Change Letter in the mail. There are changes to Medicare coverage every year, from premiums and deductibles, to levels of coverage. The Medicare Annual Notice of Change Letters are sent out annually by Medicare informing you of what changes will take place beginning January 1st, 2022. Medicare has many different programs, so not every change affects everyone – but there are some key points that we recommend checking off for any letter you get from Medicare. In this blog post, we’ll go over what to know about your Medicare Annual Notice of Change Letter!
What Is an ANOC Letter?
ANOC refers to a Medicare Annual Notice of Change Letter. This letter is mailed out by your Medicare plan every year in September, informing beneficiaries of certain changes pertaining to their plans. These changes can include things such as cost, benefits, and service areas. The changes are related to Original Medicare, Medicare Advantage Plans, and Medicare Part D plans.
Who Will Receive the Medicare Annual Notice of Change Letter?
If you are a Medicare beneficiary, you can expect to receive an ANOC letter in the mail. This includes anyone enrolled in Original Medicare, a Medicare Advantage Plan, or a Medicare Part D plan.
If you are enrolled in Original Medicare, you will receive an ANOC detailing changes to the Part A premium (if applicable) and deductible, as well as the Part B premium and deductible.
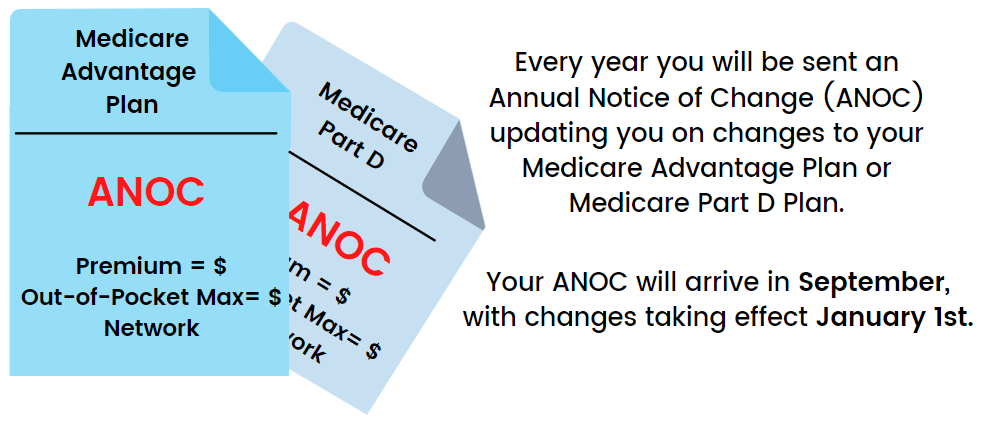
If you are enrolled in either a Medicare Advantage Plan or a Medicare Part D plan, your ANOC will come directly from the insurance company in which you are enrolled. Your ANOC will include changes to thing such as premium, benefits covered, service area, and drug formulary.
It is crucial to look over this Annual Notice of Change, as there can be large changes to your current plan for the upcoming year. Most often the ANOC is mailed with the Evidence of Coverage (EOC) for the upcoming year, which details all of the plans coverage levels.
Why Did I Receive a Medicare ANOC Letter?
ANOC letters will detail any changes in benefits for your Medicare plans. It will show if there are any changes in costs or benefits as well as any service area changes.
If you are enrolled in a Medicare advantage plan or a Medicare drug plan, the letter will come the private insurance company that administers your plan. Letters pertaining to Part A and Part B come directly from Medicare.
When Are the Changes to My Medicare Plan Effective?
 According to the Center for Medicare and Medicaid Services (CMS), the Annual Notice of Change letters are mailed every year during the month of September. This way, you are given adequate time to review the changes for the upcoming year before the Annual Election Period (AEP) beginning October 15th. If you have not received this letter by the end of September, you should contact your insurance carrier directly to confirm your address on file.
According to the Center for Medicare and Medicaid Services (CMS), the Annual Notice of Change letters are mailed every year during the month of September. This way, you are given adequate time to review the changes for the upcoming year before the Annual Election Period (AEP) beginning October 15th. If you have not received this letter by the end of September, you should contact your insurance carrier directly to confirm your address on file.
 The changes detail in the ANOC and EOC will become effective on January 1st of the following year. If you decide to change your plan during AEP due to the information in the ANOC, those changes will also become effective on January 1st.
The changes detail in the ANOC and EOC will become effective on January 1st of the following year. If you decide to change your plan during AEP due to the information in the ANOC, those changes will also become effective on January 1st.
What Are Important Things to Look for in My ANOC?
- Has the deductible for my drug plan gone up?
- Are my medications still included at the same tier levels?
- Did my monthly premium increase?
- Do I need any addition prior authorizations?
- Are my doctors and hospitals still "in network"?
- Did my out of pocket maximum change?
- Did my copays or coinsurance change?
What Do I Do if I Need to Change Plans?
If changes being made negatively affect you coverage now is the time to find alternatives. Medicare requires these letters to go out in September so you will have enough time during the Medicare Open Enrollment period to make any changes.
If you are looking to change from your Medicare Advantage Plan to a Medigap plan, it is crucial to begin the process as soon as possible, as you will need to undergo medical underwriting. This means that you will need to be health enough to be approved for a Medicare Supplement plan to begin on January 1st. Give us a call at 877-885-3484, and an experience agent will review your Medicare Supplement options, as well as walk you through the process of medical underwriting.
If you are looking to change from one Medicare Advantage Plan to another, or from one Medicare Part D plan to another, you will need to submit an application for the plan during the Annual Election Period. You must submit the application between October 15th- December 7th, and the changes will take effect on January 1st of the following year.
Understanding the Medicare Annual Election Period
AEP – also known as Open Enrollment – happens at the end of each year. You can make changes to Medicare drug plans and Medicare Advantage plans at this time. Selections must be made between October 15th and December 7th. Any changes made will be come effective January 1st. It is important to get everything done within these timelines. This would also be the time if you wanted to return to Original Medicare with a Medicare supplement.
For more information about choosing a Medicare Plan or Medicare Guides and Forms, reach out to Medicare On Video today!